Understanding OCD: More Than a Quirk or a Need for Order
We live in a world where the phrase “I’m so OCD” gets thrown around casually, usually to describe liking things tidy, colour-coded, or aesthetically pleasing. It’s said jokingly, often with pride, as if OCD were simply a quirky personality trait.
But for those who live with Obsessive–Compulsive Disorder, the reality is very different.
OCD is a mental health condition rooted in anxiety, uncertainty, and distress. It is often debilitating and time-consuming, and it can take over daily life in ways many people never see.
What OCD Really Is
Obsessive–Compulsive Disorder (OCD) is a condition characterised by:
- Obsessions – unwanted, intrusive, distressing thoughts or fears
- Compulsions – mental or behavioural rituals done to reduce anxiety or prevent imagined harm
OCD is driven by fear and uncertainty, not preference or personality. A person with OCD doesn’t wash their hands excessively because they like cleanliness. They wash because a part of their brain tells them:
“If you don’t, something terrible will happen and it will be your fault.”
Unlike a quirky habit, OCD is ego-dystonic, meaning the thoughts and behaviours go against the person’s values. They know the fear is irrational, but the anxiety feels impossible to ignore.
Intrusive Thoughts: Everyone Has Them, OCD Just Gets Stuck
Research shows that nearly everyone experiences intrusive thoughts. Examples include:
- “What if I dropped my baby right now?”
- “What if I swerved the car into traffic?”
- “What if I left the stove on?”
Most people dismiss the thought. It passes.
With OCD, the intrusive thought triggers alarm. The brain misinterprets the thought as danger, and the person feels responsible for neutralising the threat.
This is where compulsions come in.
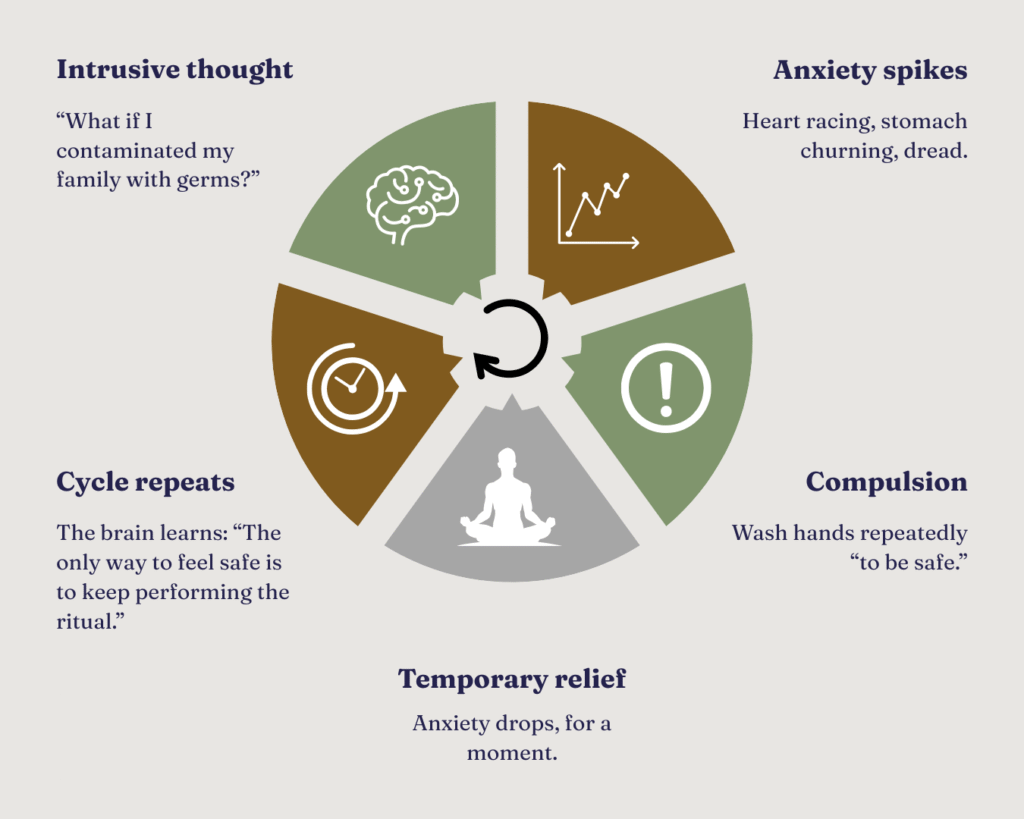
Compulsions reinforce the OCD cycle and strengthen the false belief that the intrusive thoughts are dangerous or meaningful.
OCD is Not Always Visible: The Hidden Forms
There are different subtypes of OCD, and many have no visible compulsions. These include:
- Pure O (Purely Obsessional OCD)
Obsessions occur, but compulsions are mental rather than physical.
Examples:
- mentally reviewing past events
- repeating phrases silently
- seeking reassurance endlessly
- Harm OCD
Intrusive fears about harming self or others (e.g., “What if I stab someone?”). These thoughts are not desires, they are terrifying and unwanted.
- Relationship OCD
Constant doubt about one’s relationship or partner:
- “What if I don’t really love them?”
- “What if they’re not ‘the one’?”
- Religious / Moral OCD (Scrupulosity)
Anxiety about sinning, offending God, or being a bad person.
- Sensory / Just Right OCD
An overwhelming need to repeat something until it feels “right”.

The Overlap With Anxiety, Depression, ADHD & Autism
OCD rarely exists alone. It often overlaps with generalised anxiety disorder, depression and PTSD. ADHD and autism spectrum differences (or traits) can also occur alongside OCD, contributing to overwhelm and sensory overload.
This is because all of these involve some degree of difficulty regulating thoughts, intolerance of uncertainty and heightened anxiety.
Many neurodivergent individuals, especially autistic adults or those with ADHD, also mask or hide their distress, meaning OCD can go undiagnosed for years.
Evidence-Based Treatment: What Actually Helps
OCD is highly treatable. The most effective treatment is ERP (Exposure and Response Prevention), a structured therapy that teaches the brain to tolerate uncertainty without performing compulsions.
Example:
Instead of washing hands after every intrusive thought about contamination, the person gradually learns to sit with the discomfort.
ERP retrains the brain to understand “A thought is just a thought.” Over time, anxiety drops naturally, without rituals.
Other helpful approaches include:
- CBT (Cognitive Behavioural Therapy)
- ACT (Acceptance and Commitment Therapy)
- Mindfulness-based strategies
- Psychoeducation (learning how OCD works)
Medication, such as SSRIs, can also be effective, especially when combined with therapy.
If You’re Supporting Someone With OCD
Supporting someone with OCD isn’t about providing constant reassurance or helping them complete rituals. It’s about being a calm, steady presence while they learn to tolerate uncertainty. You don’t have to fix their anxiety or argue with intrusive thoughts, simply acknowledge what they’re feeling and remind them that they’re not facing it alone.
Statements like, “I’m here, and I know this feels overwhelming,” are more helpful than trying to give solutions. Encourage professional support, celebrate small steps, and remember: recovery isn’t linear. Your consistency and compassion matter more than perfect words.
You Are Not Broken
If you’re living with OCD, the thoughts you experience can feel frightening, even shameful. But intrusive thoughts are not a reflection of who you are. They’re a symptom of a brain stuck in “threat mode.” Having these thoughts doesn’t mean you want them, agree with them, or will act on them.
Recovery isn’t about eliminating every intrusive thought; it’s about changing how you respond to them. You are not broken, defective, or hopeless. You are someone learning a new relationship with your mind; one that allows space for discomfort, uncertainty, and healing.
If any part of this resonates with you, if you’re experiencing intrusive thoughts, fear-driven compulsions, or constant anxiety, you are not alone, and you are not beyond help.
Your brain is trying to protect you. It simply learned the wrong way to cope.
Change is possible.
Recovery is possible.
You deserve a life not ruled by fear.
If you’re ready to explore support…
If OCD is impacting your daily life, relationships, or sense of safety, reach out.
You don’t have to navigate this alone.Email me at info@nnpsychology.co.uk or call 07341 193858 to learn how I can support you or a loved one move from surviving to living.