
Mental Health Challenges in a Neurodivergent World
The conversation around neurodiversity has grown louder in recent years, and rightly so. Increasing awareness of conditions such as autism, ADHD, dyslexia, dyspraxia, and Tourette’s has helped many people feel seen and validated. The neurodiversity movement reminds us that differences in how our brains work are not deficits but variations of human experience.
And yet, living in a world largely designed for neurotypical minds brings unique challenges. While being neurodivergent does not automatically mean someone will struggle with their mental health, the reality is that many do. Higher rates of anxiety, depression, and trauma have been reported in neurodivergent communities, not because of their neurology itself, but because of the environments, systems, and misunderstandings they encounter.
This article explores the intersection of neurodiversity and mental health, highlighting common challenges, systemic barriers, and most importantly, the ways forward in creating a world that is kinder, more inclusive, and more supportive of all minds.
Understanding Neurodiversity
The term neurodiversity was coined in the late 1990s by sociologist Judy Singer. It reflects the idea that neurological differences are a natural and valuable part of human diversity, rather than something inherently pathological. Just as biodiversity enriches ecosystems, neurodiversity enriches societies.
Neurodivergent individuals may experience differences in communication, sensory processing, executive functioning, and emotional regulation. While these differences can come with unique strengths such as creativity, focus, innovation, or resilience, they can also lead to struggles when societal structures are rigid, inaccessible, or intolerant of difference.
Understanding neurodiversity through this lens is essential. When we view differences as deficits, stigma and exclusion grow. When we recognise them as variations, we open the door to empathy, acceptance, and genuine support.
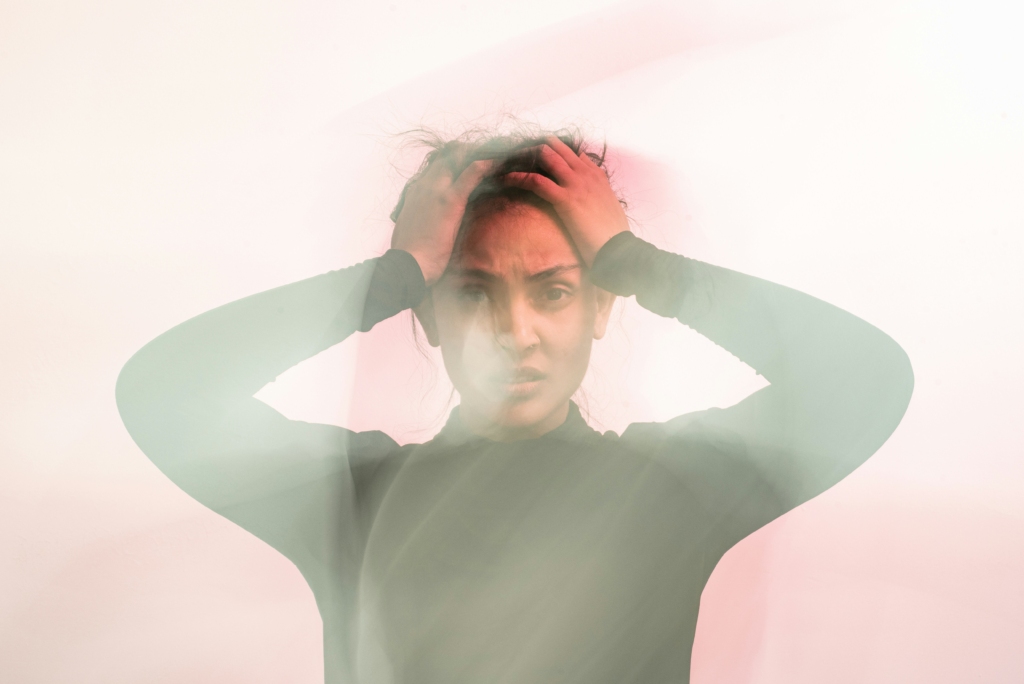
The Weight of Masking
One of the most significant mental health challenges for neurodivergent people is masking. Masking is the act of consciously or unconsciously suppressing or camouflaging one’s natural traits in order to fit into neurotypical environments.
For an autistic person, masking might mean forcing eye contact, mimicking social behaviours, or hiding sensory distress. For someone with ADHD, it might mean overcompensating with hyper-organisation or pretending to concentrate when their mind is racing. While masking can help someone survive in the short term at school, at work, or in social spaces, the long-term effects are draining.
Research has shown that chronic masking is linked to anxiety, depression, and burnout. It can also lead to a painful sense of disconnection from oneself: “If I am only accepted when I hide who I really am, do people truly care about me?” This erosion of identity can have profound mental health consequences, particularly when combined with the exhaustion of sustaining the mask day after day.
Emotional Dysregulation and Self-Esteem
Many neurodivergent individuals experience intense emotions. ADHD, for example, is often associated with difficulties regulating feelings of frustration, sadness, or excitement. For autistic individuals, the challenge may lie in processing overwhelming sensory and emotional information at the same time.
Unfortunately, society often misinterprets these differences. A child who has meltdowns may be labelled as “naughty.” An adult who reacts strongly may be dismissed as “too much.” Over time, these misinterpretations can chip away at self-esteem, leaving people feeling ashamed of their natural responses.
The reality is that emotional intensity is not a character flaw. It is a neurobiological difference. When reframed with understanding, what looks like “overreaction” can also be seen as passion, authenticity, and deep attunement to experience. Without that reframing, however, the risk of internalised shame and poor mental health grows.
Sensory Overload and Daily Stress
Another significant mental health challenge for neurodivergent people is sensory overload. Environments that neurotypical individuals might consider “normal,” such as a noisy office, fluorescent lights, crowded public transport, can be deeply distressing for those with heightened sensory sensitivities.
Chronic sensory stress can contribute to anxiety, fatigue, and even physical symptoms. If you are constantly bracing against overwhelming input, it is harder to relax, focus, or feel safe. This sense of being “on edge” can also increase vulnerability to mental health conditions over time.
For some, the stress of sensory overload is compounded by the lack of understanding from others: “It’s just a bit of noise,” or “You’re being dramatic.” This invalidation deepens isolation and can discourage individuals from seeking help or advocating for themselves.
The Double Burden: Stigma and Exclusion
Perhaps one of the heaviest weights neurodivergent people carry is the stigma that still exists around their experiences. Misconceptions, such as the belief that autism means lacking empathy, or that ADHD is simply laziness, continue to shape public perceptions and policies.
These stereotypes not only marginalise individuals but also create systemic barriers. Neurodivergent people are more likely to face unemployment, underemployment, or unstable work, even when highly skilled. They are at increased risk of bullying in schools, discrimination in the workplace, and dismissal in healthcare settings.
All of this exclusion has direct consequences for mental health. Being shut out of opportunity, misunderstood, or undervalued can lead to feelings of worthlessness, hopelessness, and despair. Importantly, these outcomes are not inevitable results of neurodivergence. They are consequences of a world that has not yet adapted.
Co-Occurring Mental Health Conditions
Research consistently shows higher rates of co-occurring mental health conditions in neurodivergent populations. For example:
- People with ADHD are at greater risk of developing anxiety, depression, and substance use disorders (Kandi and Jha 2023)
- Autistic individuals report higher rates of suicidal thoughts and self-harm compared to neurotypical peers (Newell et al. 2023)
- Dyslexic and dyspraxic individuals may experience heightened anxiety due to repeated negative educational experiences (Deighton et al. 2020, Harrowell et al. 2017)
It is crucial to note that these mental health challenges often stem not from the neurodivergence itself but from unmet needs, lack of support, and systemic barriers. Early recognition and intervention can make a significant difference, but many people slip through the cracks because services are not tailored to neurodivergent presentations.

Towards a More Inclusive World
So how can we create environments that support neurodivergent mental health rather than harm it? Change must happen at multiple levels:
- Education
Schools need to embrace neurodiverse teaching styles, reduce reliance on punitive behaviour management, and focus on strengths as much as challenges. - Workplaces
Employers must recognise the value of neurodivergent talent and implement inclusive practices—flexible working, sensory-friendly environments, clear communication. - Healthcare
Clinicians should be trained in neurodiversity-affirming practice, avoiding stereotypes and validating lived experiences. - Society
On a broader level, we need to shift cultural narratives: moving away from deficit-focused language and towards acceptance, accommodation, and respect.
Mental Health and Neurodiversity Belong Together
The intersection of neurodiversity and mental health is complex, nuanced, and deeply human. While neurodivergent individuals face disproportionate challenges, these are not inevitabilities. They are the result of systems that fail to adapt, environments that overwhelm, and cultures that misunderstand.
A neurodivergent world is not something to be “fixed.” It is something to be embraced. By fostering acceptance, reducing stigma, and creating inclusive structures, we can not only protect mental health but also unlock the richness of perspectives, creativity, and resilience that neurodivergent people bring.
To care for neurodivergent mental health is to affirm that all minds matter, and that no one should be left behind simply because their brain works differently.
If anything in this blog resonates with you, know that you don’t have to navigate it alone.
Email us at info@nnpsychology.co.uk or call 07341 193858 to learn how I can support you or a loved one on the journey toward understanding, growth, and better mental health.
References:
1. Deighton, J., Gilleard, A., Cortina, M., & Woodman, J. (2020). Dyslexia and allied reading difficulties and their relationship with mental health problems: A rapid review of evidence. UCL/Anna Freud Centre for the NIHR Children and Families Policy Research Unit. https://doi.org/10.5522/04/XXXX
2. Harrowell, I., Hollén, L., Lingam, R., & Emond, A. (2017). Mental health outcomes of developmental coordination disorder in late adolescence. Developmental Medicine & Child Neurology, 59(9), 973–979. https://doi.org/10.1111/dmcn.13469
3. Kandi, R., & Jha, S. (2023). Anxiety disorders in adult ADHD: A frequent comorbidity and a risk factor for externalizing problems. Journal of Affective Disorders, 329, 362–370
4. Newell, V., Phillips, L., Jones, C., Townsend, E., & Richards, C. (2023). A systematic review and meta-analysis of suicidality in autistic and possibly autistic people without co-occurring intellectual disability. Molecular Autism, 14, 12. https://doi.org/10.1186/s13229-023-00544-7


